One day you wake up, go about your day, and realize exercise feels different.
Your pace is slower even though you’re training the same. Your sleep is off, your mood is odd, and some mornings your joints feel older than you are.
If that sounds familiar, you might just be entering perimenopause.
Perimenopause is the transition leading up to menopause, when estrogen and progesterone begin to fluctuate. For most women, it starts in their 40s — sometimes earlier — and it can really be a confusing stage. Your cycles may become irregular, energy can change unpredictably, and what used to feel easy in training might suddenly feel harder.
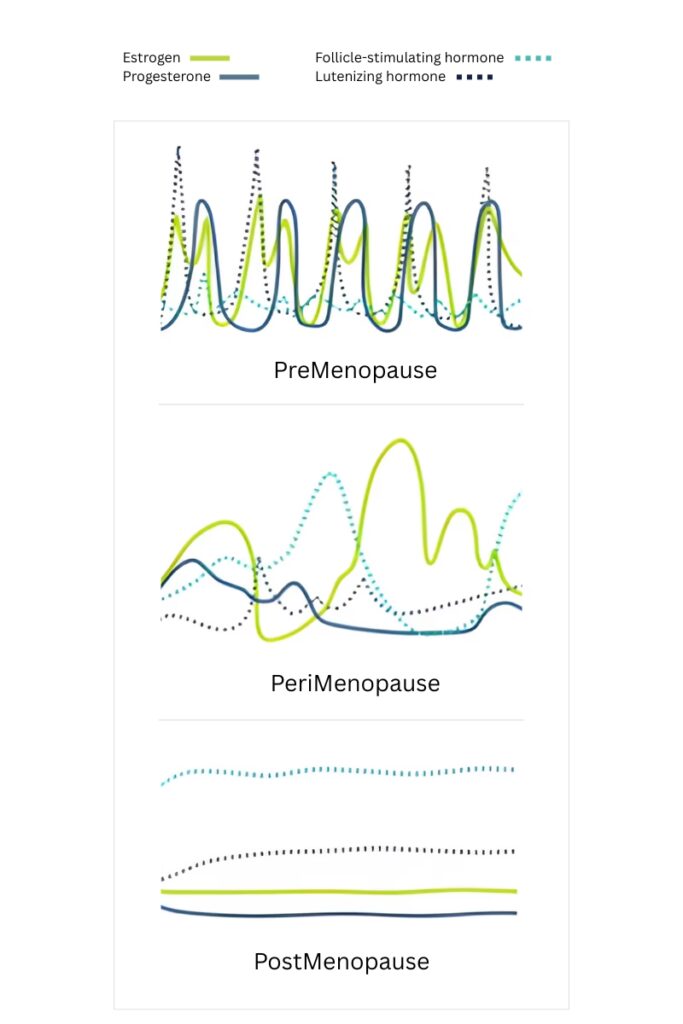
It’s also important to understand that perimenopause is more than just a hormonal rollercoaster — it also marks the beginning of increased health risks. As estrogen levels decline, women may start to experience changes in body composition (like more abdominal fat), reduced insulin sensitivity, higher blood pressure, and increased risk of cardiovascular issues. Bone density and muscle mass can also begin to decrease, and sleep disturbances or mood changes may become more frequent.
The good news is, staying active is one of the best ways to protect your health during this transition so you should absolutely keep (or start) exercising. You may just need to adjust your approach to training, recovery, and mindset (Hulteen, Marlatt, Allerton, & Lovre, 2023).

How Perimenopause Can Affect Running
With so many changes happening in your body, it’s almost impossible for your running not to be affected.
Sleep struggles
Hot flashes, night sweats, or just plain restless nights can leave you feeling tired before you even lace up your shoes. That fatigue can affect your whole day, your running workout, and your recovery afterwards.
Energy highs and lows
Some days you’ll feel unstoppable; other days, your legs may feel like concrete. These dips often come from hormonal changes and are not a sign you’re losing fitness. But it is something you need to accept and adjust to so you won’t be incredibly frustrated every time.
Aches and pains
With less estrogen protecting your joints, you may notice more stiffness — especially in the morning or after hard runs. Recovery may take longer, so listening to soreness matters.
Temperature swings
Hot flashes and sweating can make it harder to regulate body temperature on the run. Light, breathable gear and good hydration become more important now.
Mood and motivation shifts
Irritability, anxiety, or brain fog can sneak in and make getting out the door harder. Some days, just showing up is the win — and that’s enough.
How Running Can Help With Perimenopause
Running can be a game-changer during perimenopause — physically and mentally. Regular movement helps regulate hormones, stabilize blood sugar, and improve insulin sensitivity, which can reduce the weight gain around your waist that many women notice at this stage. It keeps your heart strong and helps lower blood pressure, which matters even more as the risk of heart disease rises when estrogen levels drop.
Running helps your body hang on to lean muscle, which keeps your metabolism steady and your bones supported. The impact from each step also stimulates your body to keep building bone. This slows down the natural bone loss that happens with age.
And then there’s what running does for your mind. Running triggers endorphins and other feel-good brain chemicals that can lift your mood, clear the mental fog, and take the edge off anxiety (Hulteen et al., 2023). Many women also find that regular running helps them sleep more deeply, which can make everything else feel easier to handle.

And while running is a great workout on its own, strength training is equally important, especially during perimenopause and beyond. It protects your joints, maintains muscle and bone mass, and makes you a more resilient runner. Around this stage, joints, muscles, and bones naturally lose strength — and strength training is the single best way to slow, or even reverse, that process.
Adapting Your Training
This stage of life is a masterclass in flexibility. Some days you’ll feel strong and full of energy. Take advantage of it and use your energy for a harder session on these high-energy days. Other days, your body might feel heavy, your sleep might have been interrupted, or your motivation might be off — and that’s when it’s perfectly okay to ease off, slow down, or even rest. Running by feel, rather than being glued to a specific pace or heart rate, can help you stay in tune with what your body needs on any given day and help you stay motivated.
Recovery
Recovery becomes even more important in your 40s and beyond. Your body needs more time to rebuild and recharge. Good sleep, regular stretching or mobility work, and low-stress days all play a role in helping you train consistently without burning out. Some days you may feel unusually sore, stiff, or drained after a run. That’s your body asking for a bit more recovery time — and that’s okay, too. It’s worth listening and easing up so you can come back stronger.
Strength training
And here I go again with the strength training – strength work is no longer optional — it’s essential. As estrogen drops, muscle and bone need extra support. Lifting weights, using resistance bands, or even bodyweight exercises twice a week can protect your joints, keep your metabolism strong, and make you a more resilient runner.

Balance + Agility
A little balance training goes a long way. Simple moves like standing on one foot, heel-to-toe walks, or using a balance pad can keep coordination sharp and help prevent falls or missteps on the run.
Mix It Up
Don’t get stuck doing the same run every day. A mix of easy runs, longer efforts, and some faster intervals or hill sprints will build strength and fitness more efficiently. Just make sure to sprinkle in enough recovery days so your body can adapt. Trail runs can also add variety and keep things fun.
Above all, stay open and curious. Your body is changing, and that means your training may need to evolve along with it. Running through perimenopause isn’t about doing less, it’s about doing things differently.
References
Hulteen, R. M., Marlatt, K. L., Allerton, T. D., & Lovre, D. (2023). Detrimental changes in health during menopause: The role of physical activity. International Journal of Sports Medicine, 44(6), 389–396. https://doi.org/10.1055/a-2003-9406

